Prescription drugs can be an important part of managing your health. Understanding your drug benefits makes it easier to talk with your doctor about the most effective and affordable drugs covered under your plan.
Are my drugs covered?
When your doctor prescribes a medicine, it is important to know if it is covered by your plan. The list of covered drugs is called a formulary. Your plan's formulary includes brand-name and generic drugs, biologics and biosimilars. The complete list consists of drugs taken by mouth and drugs that are injected.
Independent Health partners with doctors and pharmacists from our community to manage our formularies. Together, we review each medicine based on safety, unique qualities, how well it works and cost.
The first step is to find the name of your plan’s formulary.
- Log in to your MyIH account. Some members will find the name of their plan’s formulary on the Benefits page; or
- Your plan’s formulary name might be on your member ID card, but not all plans include this information on the card.
Need help? Contact Member Services to ask which formulary your plan uses.
After you know the name of your formulary, you can always find the latest version on our website. However, some members may find their formularies on the Pharmacy Benefits Dimensions website, a subsidiary of Independent Health.
Your formulary is organized into categories to make it easier to find what you need. It also has a guide, like a map key, that helps explain your prescription drug benefits.
Independent Health sorts drugs into cost levels, called tiers. The tier for each drug is shown on your formulary. Tier 1 drugs have the lowest cost to members. Cost can increase as the tier increases.
What are my options if my drug isn’t covered or is too expensive?
There could be a medicine under a different name that offers similar health benefits at a lower cost. Talk with your doctor to review your options, which might include the following:
Ask for a drug that is covered.
If your drug isn’t on the formulary, or list of covered drugs, show the formulary to your doctor. There might be a covered drug that is just as effective and safe, costs less or may not require prior authorization.
Most of the time, a formulary drug will cost you less than a non-formulary drug. Understanding your drug coverage and talking about options with your doctor may lower your out-of-pocket costs.
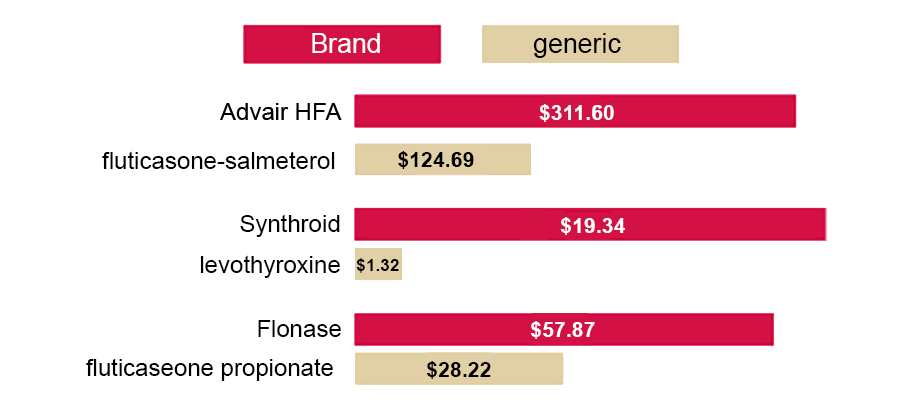
Consider a generic drug.
Generic drugs can often save you money. Ask if there’s a generic version of your brand-name medicine. Check your formulary to make sure the generic is covered.
A brand-name drug is the original version made by the company that created it. These companies spend money on research and development of the drug and have conducted costly studies to test safety and effectiveness. Brand-name drugs are usually patented and more expensive.
Once the patent expires for a brand-name drug, a generic version of the drug may become available. The generic drug is thoroughly reviewed and approved by the U.S. Food and Drug Administration (FDA), just like the brand-name drug.
A generic drug has the same active ingredient, strength and intended use as the brand-name drug. It works the same way in your body as the brand-name drug and has the same risks and benefits. However, the generic drug could have a different color, shape, size or inactive ingredient.
It is a myth that generic drugs don’t work as well as brand-name drugs. They are all tested for safety and effectiveness. Understanding this should make you feel confident about taking a generic version of a brand-name drug. Generic drugs save consumers billions each year at retail pharmacies.
BRAND vs. GENERIC *
cost estimate per month
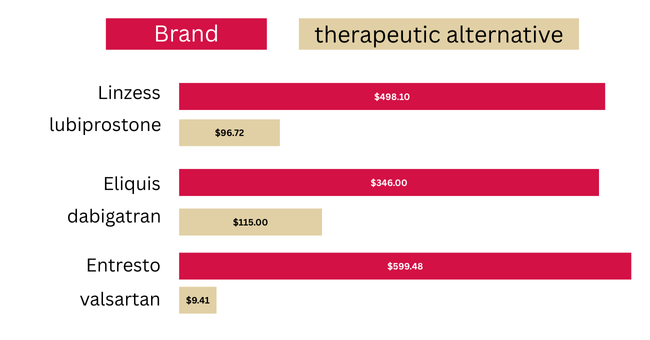
Consider a different drug.
Some brand-name drugs don’t have a generic version. However, your doctor might suggest a different brand-name or generic drug that is covered and costs less.
The alternative medicine might be listed in a different category on your formulary or have different ingredients, but it can still be approved and recommended to treat your condition.
Drug vs. Therapeutic Alternative*
cost estimate per month
Shop around.
Prescription drug prices can vary between pharmacies, just like other things we buy. Taking time to compare prices might help you save money.
If you are concerned about drug cost, call or visit other pharmacies in your plan’s network that are convenient for you. The pharmacy staff will be able to tell you the out-of-pocket cost of your drug based on your plan.
Here are step-by-step instructions to find other pharmacies in your network or make the switch to a new pharmacy.
Contact Member Services if you need assistance.
* Drug costs shown are estimates for informational purposes only and may change daily. Talk with a pharmacist for specific costs that apply to you.