UnitedHealthcare® Shared Services
Provider Resources
Access to UnitedHealthcare® Options PPO Network for Independent Health members. In December 2023, certain Independent Health products will include access to the UnitedHealthcare Options PPO network for primary and travel coverage. Access and eligibility depend on the product and member’s effective date.
How to Identify an Eligible Independent Health Member
Verify the member’s coverage and ability to use the UnitedHealthcare Options PPO network by checking the member’s Independent Health ID card. If the UnitedHealthcare Options PPO logo appears on the front or back of the card, member is eligible for benefits when accessing care outside of the Independent Health service area.
- Commercial Members
- Self-Funded Members
UnitedHealthcare Options PPO used as Primary Network
PPO/Primary Network:
- Independent Health logo on the front
- UnitedHealthcare Options PPO logo on the front
UnitedHealthcare Options PPO logo on the front
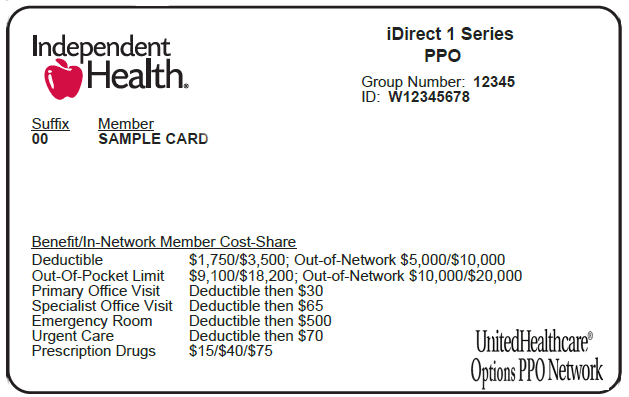
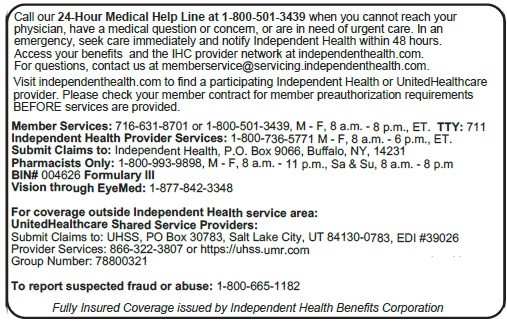
- /content/dam/independenthealth/provider/unitedhealthcare/images/uhc-commercial-id-local-front.png
- /content/dam/independenthealth/provider/unitedhealthcare/images/uhc-commercial-id-local-back.png
UnitedHealthcare Options PPO used as Out-of-Area/Travel Network
PPO/Travel Benefit:
- Independent Health logo on the front
- UnitedHealthcare Options PPO logo on the back
UnitedHealthcare Options PPO logo on the back
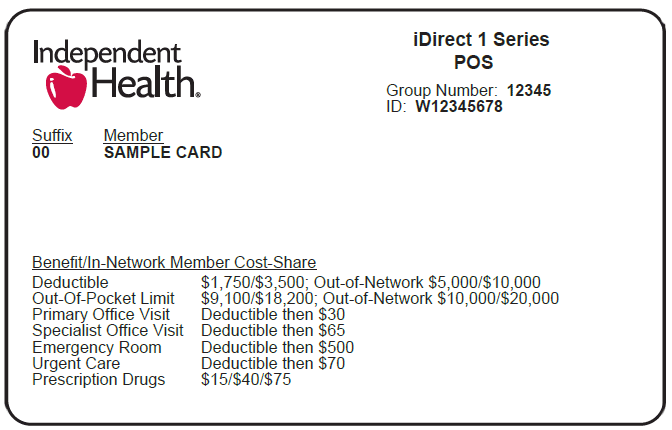
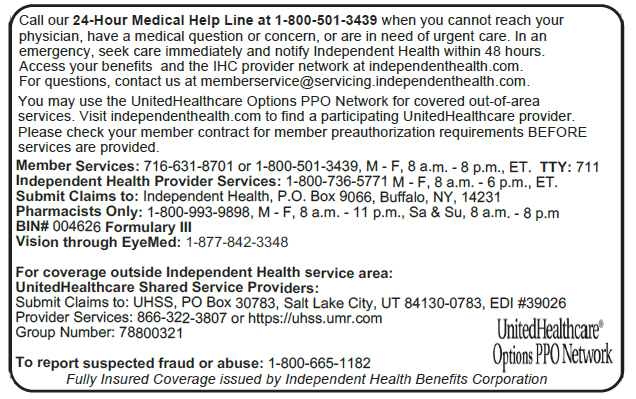
- /content/dam/independenthealth/provider/unitedhealthcare/images/uhc-commercial-id-nat-front.png
- /content/dam/independenthealth/provider/unitedhealthcare/images/uhc-commercial-id-nat-back.png
UnitedHealthcare Options PPO used as Primary Network
- Independent Health Self-Funded logo on the front
- UnitedHealthcare Options PPO logo on the front
UnitedHealthcare Options PPO logo on the front
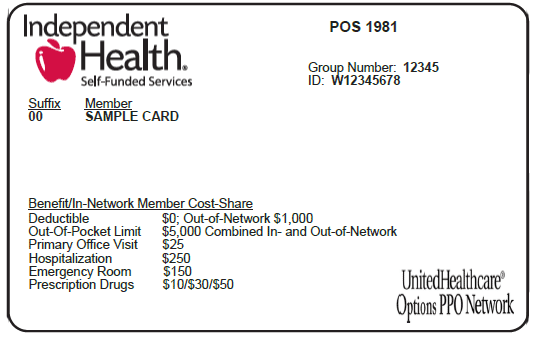
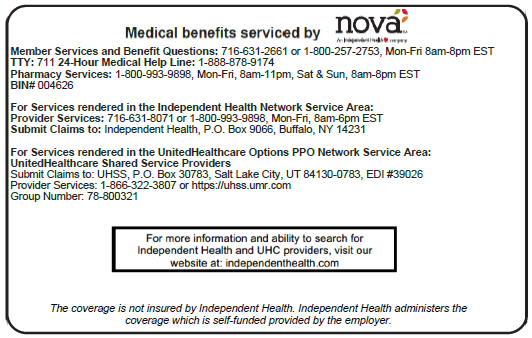
- /content/dam/independenthealth/provider/unitedhealthcare/images/uhc-sf-id-local-front.png
- /content/dam/independenthealth/provider/unitedhealthcare/images/uhc-sf-id-local-back.png
UnitedHealthcare Options PPO used as Out-of-Area/Travel Network
- Independent Health Self-Funded logo on the front
- UnitedHealthcare Options PPO logo on the back
UnitedHealthcare Options PPO logo on the back
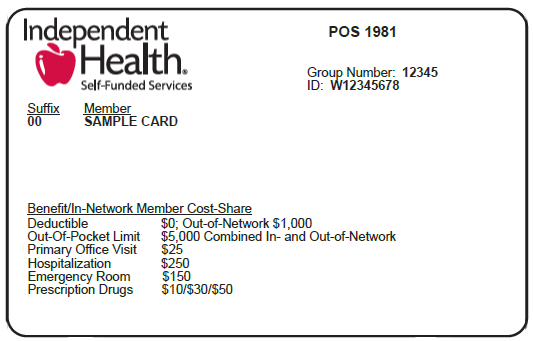
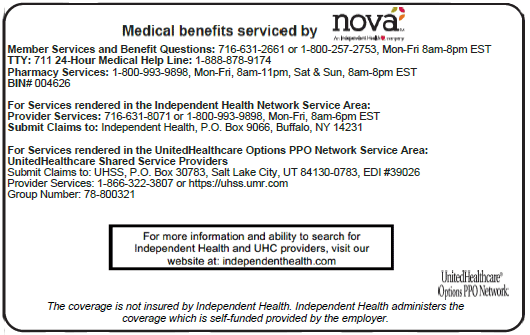
- /content/dam/independenthealth/provider/unitedhealthcare/images/uhc-sf-id-nat-front.png
- /content/dam/independenthealth/provider/unitedhealthcare/images/uhc-sf-id-nat-back.png
Commercial Fully Insured Forms
UnitedHealthcare Provider use only. Use to lodge a written appeal of an adverse determination on behalf of a Commercial Member.
Genetic Testing Authorization Request Form
UnitedHealthcare Provider use only. Complete this form to request genetic testing authorization for Commercial Members.
UnitedHealthcare Provider use only. Complete this form to request home health care for Commercial Members.
Non-Emergent Transportation Request
UnitedHealthcare Provider use only. Complete this form to request non-emergent transportation for Commercial Members
Out of Area Transfer Request Form
UnitedHealthcare Provider use only. Complete this form to request to transfer to an out of area facility for Commercial Members.
Pharmacy Drug Authorization Form
UnitedHealthcare Provider use only. Complete this form to request pharmacy drug authorization for Commercial Members.
Prior Authorization Request Form Commercial
UnitedHealthcare Provider use only. Complete this form to request prior authorization for Commercial Members.
Skilled Nursing Prior Authorization Form
UnitedHealthcare Provider use only. Complete this form to request skilled nursing prior authorization for Commercial Members.
Self-Funded Insured Forms
UnitedHealthcare Provider use only. Used to submit a written appeal of an adverse determination on behalf of a Self-Funded Member. Please note this form must include the member's signature.
Pharmacy Drug Authorization Form
UnitedHealthcare Provider use only. Complete this form to request pharmacy drug authorization for Self-Funded Members.
Prior Authorization Request Form Self-Funded
UnitedHealthcare Provider use only. Complete this form to request prior authorization for all applicable services for Self-Funded Members.
Drug Formularies
Independent Health Drug Formularies are lists of drugs that are covered under the member’s plan. Some drugs may appear on different tiers depending on the formulary.
These formulary drugs are recommended by the Independent Health Pharmacy & Therapeutics Committee. These drugs are selected based on a quality evaluation of safety, effectiveness, unique qualities, and costs.
UnitedHealthcare Provider Services
For questions related to member eligibility, claims submissions and status, authorization status and appeal status, please contact UnitedHealthcare Provider Services.
About Independent Health
Established in 1980, Independent Health is an independent, not-for-profit health plan headquartered in Buffalo, New York. In all, Independent Health and its affiliates serve a total of more than 550,000 lives across the country.
Find out more about Independent Health.