Women’s Preventive Services: Contraceptive Methods and Counseling Coverage for Members of Religious-Affiliated Employers
Federal and state legislation provides coverage for FDA-approved contraceptive services, devices and prescription drugs.
Because religious-affiliated organizations may decline to include this expanded coverage in their benefits, coverage for contraceptive services, devices and drugs is available to individuals through separate benefits.
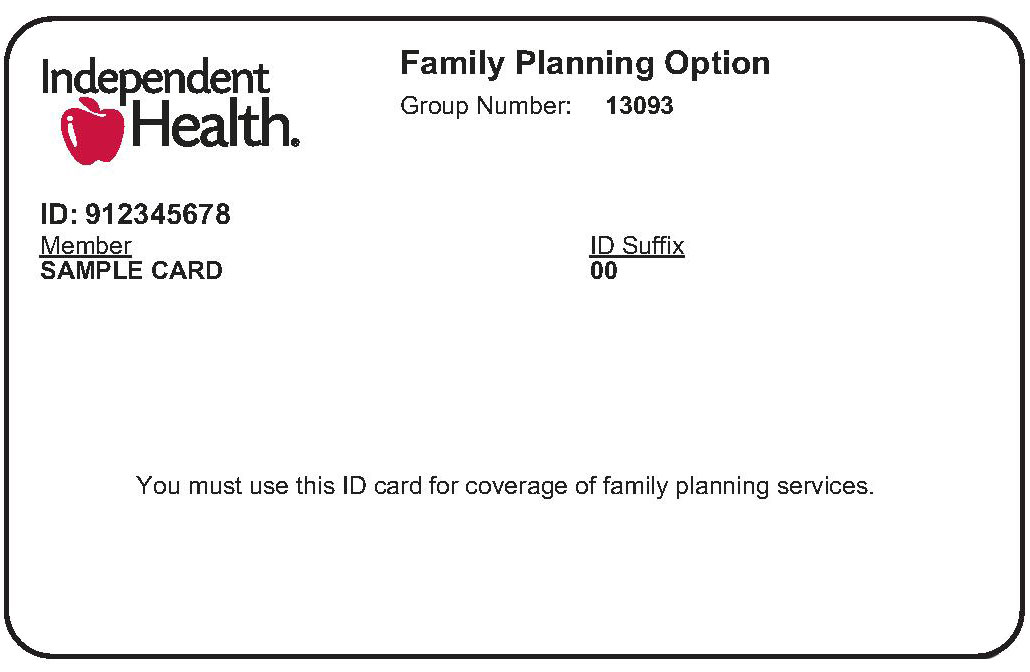
Individuals who choose this coverage receive a separate ID Card that indicates either “Women’s Wellness” or “Family Planning.” These terms are different based on the size of the group.
What's Covered:
All Food and Drug Administration approved contraceptive methods, sterilization procedures, and patient education and counseling for all women with reproductive capacity, such as:
- Sterilization Surgery
- Sterilization Implant
- Implantable Rod
- Intrauterine Device (IUD)
- Injections
- Oral Contraceptives
- Contraceptive Patch
- Vaginal Contraceptive Ring
- Cervical Cap
- Diaphragm
- Sponge
- Female Condom
- Emergency Contraceptive Pills
Patient Cost Share:
For services rendered at physician’s office or at a facility:
The cost share is different between large group and small group plans.
To verify eligibility and cost share for these services in HEALTHeNET, enter the patient’s ID number that appears on her Women’s Wellness or Family Planning card to view plan benefits.
At the pharmacy:
Generic drugs and brand-name drugs without a generic equivalent will be covered in full. Tier 3 brand name drugs with a generic alternative will be subject to the applicable plan participant copay. All prescriptions need to be filled at a participating pharmacy.
Claims Processing and Submission:
For religiously affiliated organizations that have declined coverage for contraceptive services, devices and prescriptions, Independent Health has issued a separate Women’s Wellness or Family Planning ID card. This ID card has a separate member ID number for the female members.
Facilities, physicians and providers:
- Submit claims using the member’s ID number that appears on the card labeled Women’s Wellness or Family Planning
Note: Services related to women’s preventive care, such as annual physicals, preventive screenings (mammograms, lab screenings, etc.) are covered by the female member’s health plan. Submit claims for these types of services using the member’s ID number that appears on her regular plan ID card.
Pharmacists:
- Submit claims for covered contraceptive drugs and devices using the patient’s Plan ID number that appears on the card labeled Women’s Wellness or Family Planning
- All other prescriptions should continue to be processed using the patient’s Plan ID number on her regular plan ID card
- Patients with current prescriptions for contraceptive drugs that have refills remaining do not need a new prescription.
- A prescription is required for all contraceptive drugs and devices, including covered over-the-counter items.
Questions?
Provider Relations:
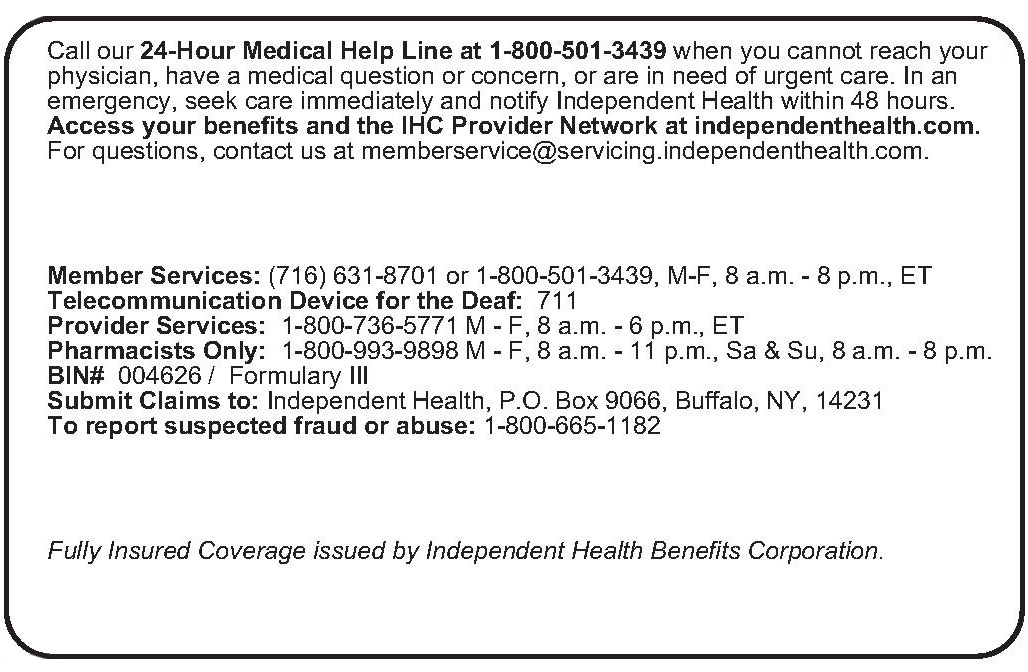
Call (716) 631-8071 or 800-862-4728, Mon. through Fri., 8 a.m. to 5 p.m.
Pharmacies:
Call 800-993-9898, Mon. through Fri. 8 a.m. to 11 p.m.; Sat. & Sun. 8 a.m. to 8 p.m.
BIN # 004626
Submit claims to: Independent Health, P.O. Box 9066, Buffalo, NY 14231
Content Updated: 2/2022